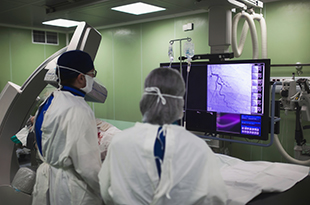
While some studies suggest female patients treated by female physicians have better outcomes, there does not appear to be a relationship between operator and patient gender and outcome in patients undergoing coronary angioplasty or stenting. These are the results of a first-of-its-kind study by the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) and published in Catheterization and Cardiovascular Interventions.
The study looked at procedures performed by 385 male interventional cardiologists, and 18 female interventional cardiologists at 48 non-federal hospitals across the state of Michigan. Female interventional cardiologists continue to be markedly under-represented and only perform a small percentage of cases, with women accounting for only 4.5% of interventional cardiologists and performing only 3% of procedures.
Despite interventional cardiology remaining an overwhelmingly male-dominated specialty, female physicians in this field stand out as excellent practitioners. Coronary angioplasties done by female physicians were more frequently rated as appropriate as compared to procedures performed by their male counterparts, among those studied. Female interventional cardiologists also more frequently prescribe recommended medical therapies than male interventional cardiologists. No differences in death, kidney injury, major bleeding or blood transfusions were found between patients treated by male or female interventional cardiologists.
“While the overall care processes and outcomes in Michigan were great, and similar for operators of either sex, the female physicians scored higher on appropriateness and post-procedural therapy. These findings would benefit female trainees who are considering interventional cardiology but are concerned about perceived barriers,” says the lead author of the study, Prasanthi Yelavarthy, MD.
The study senior author, Hitinder Gurm, MD Director of BMC2, said, “It is embarrassing that the ratio of women to men in our field remains so low in 2021. I hope that these findings will push our professional societies and training programs to develop strategies to encourage future female trainees to pursue a career in interventional cardiology.”
BMC2 is a collaborative consortium of health care providers in the State of Michigan comprised of three statewide quality improvement projects:
- A prospective multicenter statewide registry of consecutive percutaneous coronary interventions (BMC2 PCI).
- A prospective, longitudinal multicenter statewide registry of vascular surgeries and carotid interventions (BMC2-Vascular surgery).
- Michigan TAVR, a structural heart quality improvement initiative focused on transcatheter aortic valve replacement in collaboration with the Michigan Society of Thoracic and Cardiovascular Surgeons.
All projects are designed to improve quality of care and patient outcomes. The collaboration across BMC2 overcomes the barriers of traditional market and academic competition. All projects collect, audit and organize data and report procedural variables and outcomes to individual operators and institutions.
Support for BMC2 is provided by Blue Cross and Blue Shield of Michigan and Blue Care Network as part of the BCBSM Value Partnerships program.